(4 of 5)
REJIGGERING THE SYSTEM
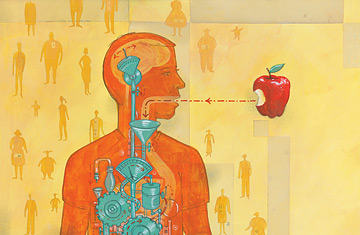
If we haven't yet figured out how to tame our need to eat, one reason may be that ghrelin, leptin and the handful of other gut chemicals are only the big dogs of the appetite-control system. Researchers have discovered at least two dozen other hormones and peptides that play a role too. Adjusting the levels of just the few we know best is a little like upgrading the quality of the gas in your car and thinking that is going to boost it from 20 m.p.g. to 75 m.p.g. You may notice some improvement, but if you really want a better, more efficient machine, you have to open the hood and retool things in a much more fundamental way. That kind of advanced work on the human metabolic engine is just what the new generation of appetite researchers is trying to do.
Carrie Haskell-Luevano, for example, an associate professor of medicinal chemistry at the University of Florida, is peering deeper into the brain, studying the receptor sites on individual neurons to which appetite-control chemicals bond. The receptor array is massively complex, with at least 40 sites known to play a role in carrying feelings of hunger or satiation and 30 more that probably do. Not all of them are created equal, however, and one of the most intriguing is what's known as the melanocortin-4 (MC-4) receptor.
MC-4 is the neural gateway for ghrelin, leptin and up to 20 other chemicals. Haskell-Luevano and other scientists have found at least 11 genetic mutations in some obese people that appear to cause the MC-4 receptor to malfunction. In some cases, the receptor may fold improperly on the surface of the cell; in others, chemicals may bond imprecisely to it. Either way, appetite regulation can get scrambled but good. "Basically," says Haskell-Luevano, "if you block the MC-4 pathway, hormones like leptin don't work."
Haskell-Luevano is also looking at the adjacent MC-3 receptor, which, while not as powerful as MC-4, does help the brain govern energy balance and can have mutations of its own. Still, genetic problems in these two receptors would not explain all cases of obesity or even very many. Only about 6% of adults and children considered obese have any MC-4 anomalies, though Haskell-Luevano suspects that other irregularities in the genetics of metabolism or appetite control could push the overall total of gene-based obesity closer to 25%.
Flier, of Harvard, is studying neurons in the hypothalamus that are supposed to produce a protein that responds to leptin but, for as-yet-unclear reasons, sometimes fail to. Find ways to stimulate those neurons—or even add doses of the protein they're failing to make—and you could theoretically restore appetite balance. And Evans, of the Salk Institute, is studying cellular receptors known as PPARs, which control the flow of sugar and fat throughout the body. After a meal, fatty acids enter cells, triggering the receptors to rev up the body's energy-burning motor. The more active this system is, the more fat you'll burn; what you don't use gets stored. If you're obese, there's a good chance your PPAR system is idling too low.
"We'd like to use a drug to boost metabolism so you're more efficient at burning," says Evans. Working with mice, he has conducted precisely those kinds of studies, developing drugs that stimulate PPARs and boost fat burning. Five pharmaceutical companies are conducting similar studies, at least two of which have now moved onto human subjects.
Another, entirely different avenue of research is being pursued by Michael Cowley, neuroscientist and associate professor of physiology and pharmacology at the Oregon National Primate Research Center. Cowley is interested in how excessive eating mirrors the patterns of drug addiction. Few people who compulsively consume—whether the substance of choice is food, drugs, tobacco or alcohol—are unaware that their habit could kill them. Yet few have the power to stop, at least not easily. "The phrase comfort food hits the nail on the head," Cowley says. In the case of both food and drugs, ghrelin again appears to play a role.
While the hormone affects three areas of the brain, it hits the mesolimbic reward region particularly powerfully. Studies of this part of obese people's brains reveal a level of activity remarkably similar to that in the brains of drug addicts when they are exposed to their preferred substance. What's more, in both kinds of people, there is a general deficit of activity in the mesolimbic region, which suggests that the compulsive intake of food or chemicals may simply be an attempt to compensate for this shortfall. Cowley has a financial stake in this argument, since he is the founder and chief scientist of a pharmaceutical company that has now moved to human trials of an antiobesity drug designed to calm the cravings in the reward pathway.