(2 of 4)
Studying such kids for more than a decade, the researchers discovered that those who became schizophrenic were most often from families that, when first interviewed, displayed "communication deviance" (unclear, unintelligible or fragmented speech) and highly critical and intrusive parenting. These weren't merely families that argued with difficult sons and daughters; they were families that had lost all ability to cope.
McFarlane and others began working with some of the families to address their interactions and teach them how to communicate better — more slowly, with less anger and intrusion. Even after they are on medication, people with schizophrenia have a difficult time tracking rapid, highly emotional speech, yet that's the kind they often hear from frustrated family members. These patients would improve in hospitals but relapse once they got home, even when they continued to take antipsychotics.
For several years, McFarlane developed and tested the Multi-Family Group approach, which brought several families together at a time to learn from one another how they sounded to outsiders. In twice-monthly sessions, the families modeled greater clarity and compassion and troubleshot daily-living problems like kids' marijuana use or sexual activity. It was a simple intervention that, when combined with antipsychotic drugs, worked to reduce schizophrenic relapse rates significantly more than the drugs alone.
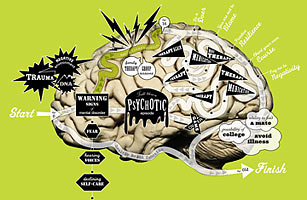
McFarlane wondered if the treatment could work even earlier, to help prevent the illness in largely asymptomatic kids who were at risk for schizophrenia. Such prediagnosis would not be easy, but McFarlane knew that once a patient's perception of reality has cracked for the first time, it becomes exceedingly hard to walk back to normality. Indeed, a major study just published in the journal Neuropsychology shows that the signature cognitive problems of schizophrenia — deficits in verbal learning and memory along with processing speed — actually begin days or weeks before a first psychotic episode, making the earliest possible detection all the more urgent.
And so in the 1980s, McFarlane began canvassing schools in the New York City area to try to get the staffs excited about preventing schizophrenia among their students. A number of the superintendents "practically threw us out the window," he says. "They just kept saying, 'We don't have mental illness in our high school.'" It was dispiriting: based on the epidemiological data, McFarlane knew that each year about 12 in 10,000 young people suffered a first episode of psychosis. Some of the kids were clearly in those schools, but if he couldn't get through the door to screen them, he couldn't prevent any illness.
A Theory Goes Wide
Even as McFarlane was exploring his schizophrenia-prevention idea, other researchers were having similar what-if moments with respect to other, more routine conditions. Suppose irritable infants who become fearful toddlers who become shy children somehow could be stopped from becoming adults with anxiety disorders. Suppose men and women who go to war or become cops in inner cities could be helped before developing posttraumatic stress disorder. Could you, similarly, identify the children of depressed parents early and give them skills to prevent their own first depressive episode?
In any given year, approximately 17% of Americans under 25 have a mental, emotional or behavioral disorder. (Over our lifetime, 46% of us will receive such a diagnosis.) If we reduce the proportion of young people who become mentally ill by even one-quarter, that would mean about 3.8 million saved each year from what can turn into a lifelong struggle.
But if most mental illnesses have a genetic origin, isn't even that modest 25%-reduction goal unlikely? The science can get tricky here, but the simple answer is that genes aren't destiny. You can't do anything to change your genome, but your environment and experiences have powerful effects on the way those genes are expressed. A susceptibility to cancer may remain just a susceptibility — until you start smoking and kick the disease process into motion. Similarly, change a child's emotional experiences for the worse and you can trigger mental illness; change them for the better and you may hush the problem genes. One concrete example of this: in 2003, a study in Science found that the larger the number of copies an individual carries of a serotonin-transporter gene called 5-HTTLPR the greater the risk of developing major depressive disorder and suicidality — but only if the individual suffers stressful early-life experiences like abuse.