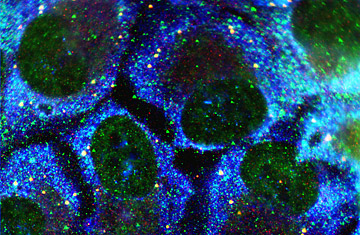
Prostate cancer cells
An experimental drug for advanced prostate cancer has shown preliminary success in the first and second phases of clinical trials, shrinking tumors in the lab and reducing signs of the disease in patients with drug-resistant cancer, according to a report published in the April 10 issue of the journal Science.
Prostate cancer, which kills 29,000 men in the U.S. each year, is a tenacious disease in advanced stages. The treatment of cancer that has metastasized beyond the prostate involves drugs that block male hormones, the androgens testosterone and dihydrotestosterone, which feed tumor growth. Antiandrogen drugs, like bicalutamide, work by binding to the androgen receptors on prostate-cancer cells, chemically preventing the hormones from interacting with the tumor. Over time, however, cancer cells become resistant to the drugs as the number of androgen receptors on the cells increases, and in a cruel twist, the drugs somehow begin to stimulate the cancer instead of suppressing it. (See the top 10 medical breakthroughs of 2008.)
Some researchers think the solution is to avoid involving androgen receptors altogether. But Charles Sawyers, a cancer researcher at the Howard Hughes Medical Institute (HHMI), isn't convinced — and he has an alternative. In the new Science paper, co-authored by Sawyers and other researchers at HHMI, the University of California, Los Angeles, and a host of other institutions, data suggest that a new chemical compound may sidestep the problem of resistance. When used to treat mouse tumors that were derived from drug-resistant prostate-cancer cells, the compound led to dramatic shrinkage, which has researchers hoping for a similar effect in humans. "The compounds are working extremely well in our models," says Sawyers. "We think this might be able to deal with the resistance question." (Read "Prostate Exams: When Are They Necessary?")
Researchers in Sawyers' lab began with a chemical that showed promise in attaching to the androgen receptor on cancer cells. Then the scientists, like composers writing variations on a theme, synthesized nearly 200 versions of the drug and screened each one on prostate-cancer cells that had been engineered to be drug-resistant. In the end, two molecules — RD162 and MDV3100 — fit the experimental criteria, binding to the receptor site without stimulating cancer-cell growth. Both chemical compounds were then tested in mice. "They caused the tumors to shrink significantly," says Sawyers.
Unlike typical antiandrogen cancer drugs, the new compounds appeared to work by more effectively blocking the androgen receptors on the cancer-cell surface, even when the total number of receptors on the cells was high, as is the case in resistance. (Read "Vitamins Do Not Prevent Prostate Cancer, Study Finds.")
The drug company Medivation, for which Sawyers is a paid consultant, chose MDV3100 to test in a clinical trial. In initial studies, 30 patients who had drug-resistant prostate cancer were given doses of MDV3100. Twenty-two showed a sustained reduction in their blood levels of prostate-specific antigen, or PSA, a protein that is elevated in the presence of prostate cancer; in 13 of those 22, the decline was more than 50%. That Phase 2 trial is ongoing, but the drug has shown enough promise to prompt the Food and Drug Administration to grant Medivation permission for a large-scale Phase 3 clinical trial of 1,200 patients with resistant prostate cancer, which will determine the drug's impact on survival rates.
That trial — needed before MDV3100 can be approved for use in humans — will take several years. In the meantime, there are still questions to be explored, including why the drug had little effect in eight of the subjects in the early clinical trial. Sawyers' team is working on an answer. It's possible that the drug may have to be given in larger doses to some patients or that some prostate cancers may mutate to the point where antiandrogen drugs are simply ineffective. "There could be changes that are preventing the drug from binding," he says. "It's a bit like trying to hit a moving target." But for now, MDV3100 offers some potential as better ammunition.
