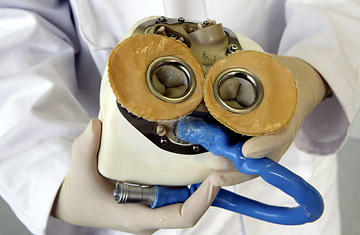
The prototype of a fully implantable artificial heart.
Working with the European Aeronautics Defense & Space (EADS) — best known as the maker of the Airbus jet — French researchers have developed a pioneering new artificial heart. Dr. Alain Carpentier, the heart surgeon who led the development of the device, said that the first heart patients may receive the experimental organ in just three years.
"This attempt to permanently replace the physiological heart with a completely new artificial heart has been the Holy Grail of researchers," says Dr. Peter Weissberg, the British Heart Foundation's medical director, who was not involved with creating the new device. "The question now is whether it can prove as durable as the natural heart by beating 60 to 100 times per minute for life."
Its developers say the new heart is the closest thing yet to the human body's natural ticker. Independent experts agree that it offers several significant improvements over what's currently available. The new device employs two pumps, instead of one, more accurately mimicking the function of a real heart's two ventricles, as well as a system of miniature sensors that react to physical activity and automatically increase or decrease the heart rate and blood pressure. The prosthesis also uses new composite bio-tech materials, which are made from animal tissue and chemically treated to eliminate the risk of blood clots, Carpentier says, a problem that has plagued earlier alternatives. (See TIME's A-Z Health Guide.)
Most earlier mechanical hearts — such as the seminal Jarvik 7 and other ventricular assist devices — were not designed to replace diseased hearts entirely, but to assist impaired function and bridge heart patients to transplant. Other total artificial hearts, meanwhile, such as the U.S.-developed AbioCor and a prototype being tested by MagScrew, have not successfully modulated beating and pulse according to the physical needs of the host.
"That physiological feedback capacity would mark a major step forward, probably allowing patients to live more normally than in the past," says Dr. Timothy Gardner, president of the American Heart Association, of the new French device .
That's good news for the estimated 20,000 people worldwide who are each year in urgent need of a heart transplant for survival. Currently, only about a quarter of those patients receive transplanted hearts from donors. The need for a viable artificial alternative is clear; if Carpentier's device proves reliable and durable, it promises to shorten transplant wait-lists and save the lives of at least some of the 17 million people who die of heart disease every year. The first transplant patients will likely be the critically ill, who currently receive existing artificial hearts as end-of-life treatments, but Carpentier expects his new heart to be tested increasingly in younger heart patients whose bodies may be in better shape to recover from an artificial-organ transplant — and resume a relatively normal lifestyle.
It's a promise has been at least 15 years in the making. Carpentier, having invented bio-engineered heart valves three decades ago, sought next to create the ultimate artificial heart. His efforts got a major boost in 1993 when the late French media and aerospace magnate Jean-Luc Lagardère and his Matra aviation group — which was later folded into EADS — offered materials and financial and technical support. Carpentier announced the final step of that collaboration last month, along with the prosthetic heart: the launch of Carmat, a new $9.2 million firm that will build and eventually market the heart. Carmat (for Carpentier and Matra) is backed by EADS and a Paris-based private equity firm called Truffle Capital, plus $33 million from a French agency funding innovation. If the marriage of cardiac research and high-tech avionics sounds quirky to some, Carpentier says it's a natural match — the durability of his artificial heart depends on some of the same materials and technologies that keep planes in the sky for thousands of high-stress hours.
So far, the Carmat heart has been tested in the lab and in animals; it could take up to two years to get the approval needed to begin human trials. Among the issues that still need to be worked out: battery life. One charge, for example, runs anywhere from five to 16 hours. Though that's significantly better than older rivals, which last just 30 minutes if disconnected from a power source, it poses the problem of frequent recharging — and methods of doing so without increasing the risk of infection. "It's obvious that a major restriction of any artificial heart is recharging the battery in it," says Carpentier, who says major advances in battery capacity are on the way. "But these prosthetic hearts are designed for people — some as young as 40 or 45 years old — who'd simply die without them. Considering the option, having to charge the battery once or twice a day is no huge trauma."
If the heart proves safe — a high bar — it's expected to hit the market with a $250,000 price tag. Some experts say that Carpentier's direction of the project provides enough reason for hope. "He is a genius in his field and an internationally respected figure, both as a developer of devices as well as a transplant specialist. Carpentier brings a lot of authority and gravitas to this," says Dr. Gardner. "Predicting success would be premature, but the fact this is Carpentier's project increases the chances it may constitute a big breakthrough."
