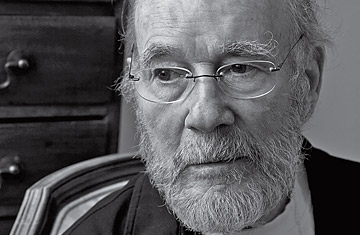
Dr. Peter Goodwin
You were instrumental in the campaign for Oregon's pioneering Death with Dignity Act. Why that issue, death?
In 1972, long before hospice existed where I practiced, I helped a man die. He and his wife came to see me. He handed me a whole sheaf of information about his condition, and he said, "Doctor, I want you to help me die." And I recoiled, but their problem was so, so pressing that I gave him a prescription. For months I was terrified. I put my own career and my family's livelihood in jeopardy.
Oregon's act basically allows mentally competent people who have less than six months to live to get medication that will hasten their demise. How is that not assisted suicide?
If you think of a typical suicide, it's impulsive, it's often violent, and it's almost always in seclusion. This is a process done with the support of the family, after a great deal of consideration. And it's a gentle death.
Does it worry you that there could be abuse? Patients could get the meds while they were lucid, but when they became a burden, someone else could administer them?
Theoretically there would be that possibility. For the most part, I've found when patients slip away in that way, the family becomes more concerned about their welfare and more likely to find help.
The only other states where patients can do this are Washington and Montana. Why hasn't it spread further?
There's tremendous opposition from the religious community, for reasons I accept. There's built-in antagonism among the medical profession. "I think I've done all I can, and I'm not going to do any more" is not the sort of thing doctors say. And patients and their families have the hugest difficulty in accepting that they are beyond treatment in a curative sense.
This legislation has become very personal to you. Why?
It's a brain disease: corticobasal ganglionic degeneration. It has caused me to lose all useful function in my right hand and a lot of the function in my left. I can no longer eat in public. My balance is gradually deteriorating. My three doctors agree that I'm within six months of dying. My attending physician has given me a prescription for medication to end my life, and I have had it filled.
How did your four children react when you told them?
They've accepted that my life is coming to an end, regretfully. We do a lot of crying.
Why not just hospice care? Why intervene?
Hospice is marvelous. But I think the patient should be in control of the process. The patient then can pick the time when family will be present and can say goodbye.
Of the 71 patients who received prescriptions last year, only one was referred for a psychological evaluation. Isn't depression an issue?
I'm sad as all get-out because I'm losing my children. Depression is very different. It's sort of an insult to make these patients see a psychiatrist.
As a doctor, is it easier or harder to make this decision?
Physicians die in a different way from the majority of their patients, long before they've had a huge amount of chemotherapy. They know what's in store, and they have an out.
What do you hope for after death?
Foremost, if I had a choice, reuniting with my wife. And I'd like to keep learning.
Goodwin ended his own life on March 11
TO SEE VIDEO OF THIS INTERVIEW, GOODWIN'S LAST, GO TO time.com/10questions
