(2 of 2)
Still, Pennington says there are lessons to be learned. He says the vaccine surplus in many cases can be ascribed in part to countries' own pre-existing pandemic-preparedness plans. Many such plans, which were put in place in the mid-2000s, were based on the worst-case-scenario assumption that the next pandemic virus would be some variation of the highly lethal H5N1 bird-flu virus, which has so far killed 263 people. The U.K.'s plan, for example, which was automatically enacted when the WHO declared the H1N1 pandemic, predicted between 50,000 and 750,000 deaths from a flu pandemic. So far, there have been 400 British deaths from H1N1.
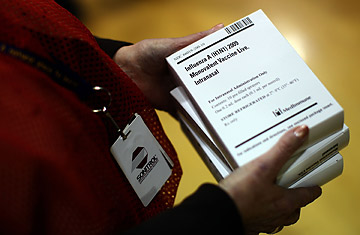
As part of their plans, many governments lined up multibillion-dollar advance-purchase agreements with pharmaceutical companies to buy vaccines during a pandemic. When the WHO declared H1N1 as such, governments were locked into these contracts, if not legally then politically — amid news reports of a new and potentially lethal virus spreading around the globe, governments could not responsibly pass on the option for vaccine. In this context, governments may have felt the only prudent course was to err on the side of caution.
Pennington says that to avoid similar situations of oversupply in the future, governments may want to plan a range of responses for the next flu pandemic, based on a virus' severity. But such evaluations of deadliness of an emerging disease are much harder to carry out than one would hope — if not impossible. And delaying action in response to an unpredictable new virus could potentially mean an increase in preventable deaths. "I think all countries recognize the desirability of flexibility in implementing pandemic plans. But exercising flexibility is really hard especially when large and complicated events like pandemics are often very confusing, and the expectations of populations can swing dramatically over short periods of time," says Fukuda.
The current glut of vaccines in rich nations may at least prove useful to the 95 countries in the developing world that have no access to vaccines, 86 of which have written to the WHO requesting help obtaining supplies. The WHO already has 200 million doses for such countries, and the first doses of that stockpile arrived in Mongolia and Azerbaijan this month. These doses will be supplemented by bilateral deals: France, for example, plans to sell 2 million vaccine doses at cost to Egypt and 300,000 to Qatar, according to a report in the Parisien newspaper.
It appears that even in developing nations, however, the need for vaccines is not overwhelming. Despite fears that H1N1 would hit developing nations hardest, the pandemic is unfolding in those countries "in a similar pattern" to that in the developed world, says Fukuda — which is to say with relatively few deaths. In fact, some developing countries, particularly in West Africa, are reporting lower rates of infection than in the developed world. "Based on the current H1N1 strain, there are higher health priorities in the developing world," says Sandra Mounier-Jack of the Communicable Diseases Policy Group at the London School of Hygiene and Tropical Medicine, citing illnesses such as HIV, tuberculosis and malaria.
Mounier-Jack's comment echoes the basic question that Wodarg and other critics of the WHO are aiming to pose at Tuesday's hearing: Given that other health problems were more deserving of the billions of dollars spent tackling H1N1, how do the WHO and governments explain their decisions?
The U.S. government, for its part, still wants to vaccinate as many people as possible against H1N1. Although it has indeed been a mild flu season so far, says Jeff Dimond, a spokesperson at the Centers for Disease Control and Prevention, "our message right now is that people should get vaccinated. We are aware that a third wave of infections is possible, so we aren't making any decision yet on whether we will use our full capacity of 251 million doses."
