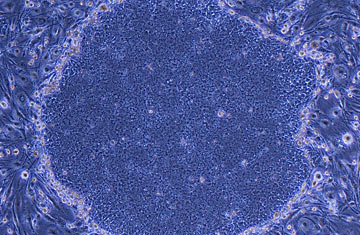
Human-induced pluripotent stem cells appear
Researchers are inching ever closer to bringing the latest stem-cell technologies from bench to bedside — and are, in the process, learning more about some diseases that long have remained medical black boxes.
This week, scientists at the Harvard Stem Cell Institute (HSCI) reported the first success in generating new populations of insulin-producing cells using skin cells of Type 1 diabetes patients. The achievement involved the newer embryo-free technique for generating stem cells, and marked the first step toward building a treatment that could one day replace a patient's faulty insulin-making cells with healthy, functioning ones.
The experiment, published in the Proceedings of the National Academy of Sciences, also provided the first good model — in a petri dish — of how Type 1 diabetes develops, giving scientists a peek at what goes wrong in patients affected by the disease. Such knowledge could lead to not only new stem-cell-based treatments, but also novel drug therapies that might improve the symptoms of the disease.
Douglas Melton, co-director of HSCI, and his team took skin cells from two Type 1 diabetes patients, exposed the cells to a cocktail of three genes that converted them back to an embryonic state — which are referred to as pluripotent stem cells — then instructed the newly reborn cells to grow into beta cells, the cells in the pancreas that secrete insulin. In Type 1 diabetes, these beta cells no longer work to break down the glucose that floods the body after each meal, leading to blood-sugar spikes that can damage the kidneys and heart.
To test whether their lab-made cells could function like normal beta cells, Melton's group exposed them to glucose in a dish. When sugar levels were high, the cells produced more of a protein that beta cells release when they break down sugar; when glucose levels were low, the protein levels were low as well.
"These cells represent the newest model of diabetes for humans," says Melton. "We have a lot of good models of Type 1 diabetes in the mouse, but everything that we have learned from them has failed in the clinic. Now we have a chance at figuring out how humans get the disease."
Diabetes researchers believe that the disorder is caused by some type of immune reaction gone awry — immune cells are "trained" in the thymus gland to recognize the body's own cells and protect them from destruction. For some reason, this education doesn't occur properly in Type 1 diabetes patients, and the immune system sees the pancreatic beta cells as foreign. Melton's team is currently working to generate thymus cells from diabetic patients in the same way the team created the beta cells, in order to put all the players together in a lab dish, in a kind of biological diorama of the disease.
The researchers are hoping to learn whether diabetes begins in the thymus or in the pancreas, where beta cells somehow change and are no longer recognized or protected by the immune system. "We still really don't know the mechanism of what causes this disease," says Melton. "We don't know which cell is initially responsible, and we don't know if certain people are destined to get it, or if there are things we can do to prevent it, or how to reverse it."
That may soon change, if the beta cells Melton created can give scientists a full picture of the disease. If, for example, it turns out that the new beta cells can be made to survive the attack by the immune system, then the next step would be to return the functional beta cells, generated through strategies like the one used by Melton, back into the patients from whom the original skin cells came. But even that won't happen until more testing is done on the cells to ensure they are both safe and effective.
One problem is that the cocktail of genes that the HSCI team used to turn back the clock on the patients' skin cells work by integrating themselves into the genome of the skin cell with the help of a virus. Such embedding of foreign matter isn't ideal for a treatment designed for the clinic, since changes in the genome could result in a variety of potential problems, including the formation of tumors and uncontrolled cell growth. Melton's group, as well as those in other stem-cell labs around the world, are working to substitute these dangerous genes and viruses with chemicals that might prove safer.
As these methods of making beta cells become more established, says Dr. Rohit Kulkarni, a diabetes expert at Joslin Diabetes Center in Boston, the strategy could be expanded to help patients with either Type 1 or 2 diabetes. "It might even be more relevant for other types of diabetes where there is no immune-system attack," he says. In those cases, simply replacing nonfunctioning beta cells might go a long way toward treating or even curing the disease.
But before that can happen, says Melton, the newly formed beta cells can become a valuable resource for understanding Type 1 diabetes better — to answer key questions such as what makes the cells so ineffective in diabetics, and whether new populations of beta cells could survive and function if transplanted into patients. "This is opening a door to a long-term project to get at the cause of this disease," he says. "But it is a new door."
