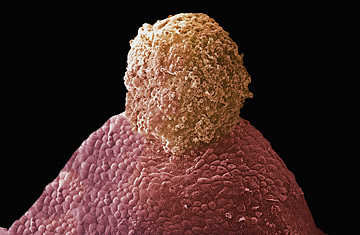
Mammalian ovulation
(2 of 2)
But using immunosuppressant therapy at all for nonlifesaving transplants lies in murky ethical territory, says Dr. Roger Gosden, director of reproductive-biology research at Cornell's Center for Reproductive Medicine and Infertility. Gosden, who did early research in ovarian transplantation in sheep and has co-authored several papers with Silber, says it's difficult to justify such drastic measures when there are so many other avenues to motherhood — adoption, surrogacy, egg donation. What's more, the prospect of a lifetime of drug therapy and its impact on the patient need to be heavily weighed, he says. "I suppose you could say, 'She could have the transplant, try to get pregnant and later have it removed, and then stop the immunosuppression.' " But that course of treatment may stretch the boundaries of what is medically ethical and reasonable for the patient. "It becomes very tricky," he says.
Tricky and possibly unrealistic, says Dr. Mitchell Rosen, director of the Fertility Preservation Center and Reproductive Laboratories at the University of California, San Francisco. "I don't think it would be used as a mainstream form of fertility treatment," he says. "I don't think it's going to replace IVF." Though he acknowledges the powerful desire to conceive the old-fashioned way, he points out that compared with the transplant process — finding an organ donor, enduring a long surgery and facing the possibility of a lifetime of drug therapy — IVF offers a simpler, more logical route. (Read "The Year in Medicine 2008: From A to Z.")
Still, fertility specialists agree that ovarian transplantation may be vital for patients suffering from life-threatening diseases. "It's a no-brainer that we should offer this to cancer patients," says Silber.
Amy Tucker, now a 31-year-old registered nurse, received a Hodgkin's disease diagnosis a little more than a decade ago. She underwent six months of initial treatment, after which the cancer recurred. Tucker was then scheduled for a bone-marrow transplant, full-body radiation and additional chemotherapy. But a couple of days before her bone-marrow transplant was to take place, a nurse practitioner happened to mention a lecture she had heard given by a local fertility specialist, Dr. Silber. Until then, Tucker had not once considered her fertility or, for that matter, anything else but the cancer treatment at hand.
Tucker subsequently had her right ovary removed and the tissue preserved. In January, a full decade later, she had her own tissue transplanted back into her body. Now, she hopes, she'll be able to bear her own children. "I haven't had a period for 10 years," she says. "But now, oh my God, I might actually be able to get pregnant."
One reason specialists urge moving toward whole-organ preservation for cancer patients is that it can be done so quickly. Tucker was able to have her ovary removed right away — unlike harvesting eggs, which can take weeks — and that meant she could begin her cancer treatment without delay. It would take another decade for Tucker to start thinking about children or reimplanting the ovarian tissue. "Basically, Dr. Silber had said, 'It doesn't matter when you put it back in. It's the ovary of a 20-year-old,' " Tucker says.
That's what makes the technique potentially appealing for other women — healthy women who simply want to delay pregnancy for lifestyle purposes. "For those who want to have children, they will often say that it is the supreme experience in their life. To deny that, or to provide obstacles when technology allows it, would be a matter of deep concern," says Gosden. Though he believes that physicians should seriously consider the ethical implications of using ovary transplants liberally to extend fertility, he says much of the debate will be decided by the would-be mothers themselves.
The primary concern, says Rosen, is the tragedy of a false promise. "You don't want to take a population and promise them something — tell them it's O.K. to wait until you're 40," he says. At 40, the transplant may not work.
Silber says without hesitation that he would help all women who wish to preserve their fertility this way — as long as patients were fully aware of the potential risks of ovary removal, which include early menopause. In fact, Silber is currently awaiting Institutional Review Board approval to perform ovary-tissue transplants for seven nonidentical twin pairs who have asked for it. (The potential transplant patients are Orthodox Jews, who for religious reasons are prohibited from using donor eggs.) He estimates that he should be able to perform the surgeries within a matter of months. "I know there will be people who have big ethical debates about it," he says, but in many ways, this seems like a logical progression of science. "Women are able to put off childbearing because of these enhanced opportunities in society and often don't seriously think about having kids until they're 35 or 40. By then, there's a 50% chance that they're infertile," he says. "Normally, we worry that science is getting way ahead of society," Silber adds. "This is exactly the opposite of that."
The original version of this article neglected to mention the context in which Dr. Silber hopes to perform ovary-tissue transplants for seven nonidentical twin pairs: to restore fertility in women whose religion prohibits them from using donor eggs. The article has been modified to include that information.
Read "Could a Common Painkiller Cut Your Risk of Ovarian Cancer?"
