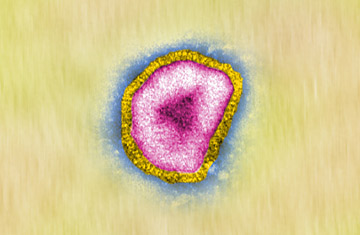
A proposed method of fighting influenza could combat the spread of avian flu, seen in the micrograph here
Many parts of the country are now sneezing, sniffling and coughing their way through yet another achy flu season. If there is any solace in the suffering, it's that so far, the Big One — the pandemic that experts predict could emerge from birds or cats or some other animal reservoir at any time — has yet to strike. (See the top 10 animal stories of 2008.)
But if it does, we might be better prepared than we ever were, thanks to a clever new strategy that scientists are testing for an improved way to treat influenza. Researchers at the Dana Farber Cancer Institute, the Burnham Institute for Medical Research and the Centers for Disease Control and Prevention have collaborated to test an antibody-based therapy for flu. Specifically, they tested antibodies that target core, conserved regions of the virus that do not mutate as readily as other parts. That's a little like attacking the virus's operating system instead of its software. Go after such primal programming, and the bug has less of a chance of mutating its way to resistance — and the vaccine may even have a chance of lasting beyond a single flu season. (Learn more about the history of the flu vaccine.)
Current flu vaccines are rejiggered every year in an attempt to keep up with rapidly adapting influenza strains. This immunological arms race is necessary because the viruses are very good at setting traps for the vaccines. The immune system is calibrated to crank out antibodies in response to the proteins it sees in the greatest quantities. Over the ages, the flu virus has thus evolved a shape like a bobble-head doll, and it covers the head portion with proteins it can easily change or do without. The vaccine targets these ever changing spots, and by the time the next season comes around, the change has been so great that the vaccine is useless. (Read "How Long Does Flu Immunity Last?")
The new strategy takes a bead on a much smaller region, closer to the soles of the viral bobble head's feet, where the virus fuses to the cell it infects. These regions mutate less rapidly, and in fact, in the recent study in mice, published in the current issue of Nature Structural & Molecular Biology, they did not mutate at all. "If we use this approach judiciously, we should be able to keep this pocket conserved and not develop drug resistance to it," says Dr. Wayne Marasco of the Dana Farber Cancer Institute, a co-author of the paper. "The exciting part is that this is really a therapy that can be used for prophylaxis and treatment."
So not only can these antibodies potentially treat an infection once it has already occurred — by disabling the viruses and preventing them from infecting additional healthy cells — they can also position themselves in the binding site of the cells themselves, blocking the virus at the receiving end too. One more advantage of this viral weak spot: it's the same on the vast majority of influenza strains circulating each year, including the ones responsible for the bird flu, H5N1. That makes this antibody approach potentially useful not only against seasonal flu but against pandemic strains as well. (See pictures of the bird flu.)
Marasco believes that if additional testing goes well, a version of the antibody therapy could be in trials as early as 2011. And with the cost of antibody therapies — currently used in cancer care and in many pharmaceutical products — going down, an actual flu treatment wouldn't be far behind. It can't come too soon.
