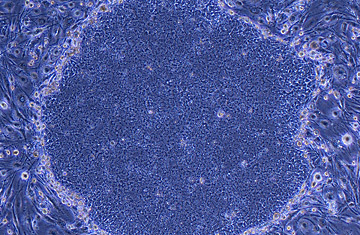
Human induced pluripotent stem cells, or iPS cells.
Correction Appended: Dec. 11, 2007
Before Dolly, no one thought it was possible to turn back time, especially where biology was concerned. Once a cell started on its march of development, nothing, absolutely nothing, scientists thought, could turn it around again. Dolly, the cloned sheep, proved this biological maxim wrong in 1996, when Ian Wilmut was able to coax an aging mammary cell to become an entirely new sheep by giving it a home in a hollowed-out egg. And since every scientific experiment just begets more experiments, Dolly's birth got researchers to wondering: If the egg can reprogram a cell, is it possible to tease out exactly what age-reversing factors the oocyte uses, and mix up a Fountain of Youth cocktail that would work on any cell without the need for an egg?
The answer is a resounding yes, as evidenced by two groundbreaking papers published on Tuesday. In the journal Cell, Shinya Yamanaka of Kyoto University reports success in turning back the clock on cheek cells from a middle-aged woman, while James Thomson of University of Wisconsin, the first to isolate human embryonic stem cells, achieved the same feat with foreskin cells from a newborn baby. The achievements completely reset the boundaries of the stem cell debate, because both groups generated cells that looked and acted like embryonic stem cells, but without the need for eggs, embryos or ethical quandaries about where the cells came from. "I think this is the future of stem cell research," says Dr. John Gearhart, the biologist who first discovered human fetal embryonic stem cells. "It's absolutely terrific."
What's more, these advances are only the latest in a year's worth of exciting firsts in the field. Earlier this month, scientists in Portland successfully nurtured a line of embryonic stem cells from monkeys using the same process that created Dolly. The feat brings us one step closer to being able to generate patient-specific stem cells to treat diseases in human patients, since primates are evolutionarily closer to humans than mice, in whom the process was tested.
The technique, however, called nuclear transfer, is a cumbersome process that requires a steady supply of high-quality donated eggs, and a deft hand to empty out the genetic contents of those eggs and replace them with the DNA blueprint from another, aging cell. The odds of success are pretty low, even in the hands of experts with years of experience.
That's why nearly every major stem cell lab began looking for an alternative approach, the most promising of which was to simply reprogram adult cells without eggs or embryos. "When I started this work, I thought it would be a 20-year, not a few-year problem," says Thomson. But sometimes science can be surprising, and in this case, all it took to accomplish a complex biological time warp was a handful of genes that suppress cells from dividing and maturing.
Already, the process, called direct reprogramming, is changing the field — on several levels. Ian Wilmut, the pioneering biologist responsible for cloning the first mammal, Dolly, has announced that he will no longer use the cloning method that made him famous to generate stem cells. "Changing cells from a patient directly into stem cells has got so much more potential," he says.
And generating stem cells is suddenly possible for anyone with a basic background in molecular biology. No special expertise in handling chromosomes, nuclei or eggs is needed.
Finally, the promise and potential of directly reprogrammed cells calls into question whether embryonic stem cells are useful any more. Why go to the trouble of creating embryos when stem cells can be coaxed directly from properly manipulated cells? At least for the time being, says Dr. Douglas Melton, co-director of the Harvard Stem Cell Institute, embryonic stem cell research should continue, since it's not clear yet how robust and safe stem cell therapies from other methods might be. "My answer to that question comes from a different perspective," he says. "Not from a scientific or political one, but from a patient perspective. A patient doesn't care how we got there. They're suffering from a disease and want to get the therapies as fast as they can. Until this method produces cells that have fully normal behavior, and normal physiological behavior, we cannot eliminate any avenue of research."
Neither Yamanaka nor Thomson believes their cells are quite ready for patients yet; for one, both methods use viruses to deliver the time-reversing genes, a practice that is acceptable in the lab but unsafe for the clinic. But the advances are finally pushing stem cell researchers to start talking about when, not if, stem-cell based therapies will be developed to treat diseases.
The original version of this story incorrectly stated that scientists in Seattle had cloned embryonic stem cells from monkeys. In fact, the scientists were working at Oregon Health & Science University in Portland.
